
Our research team developed a semistructured guide before the study. Individuals who did not respond to the initial mailings were sent another invitation. Because Spanish-speaking children make up about one-third of the pediatric population at VCUHS, we also included Spanish-speaking caregivers in this study.Ĭaregivers were contacted through direct mailings, while clinicians serving pediatric patients in VCUHS were contacted through e-mail. Well-child visits were identified by relevant International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) or International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes (eg, V20.2, Z00.129) and Current Procedural Terminology (CPT) claims codes (eg, 99381). We excluded patients without any well-child visits recorded as this group may have used a different health system as their primary care medical home. We hypothesized that using a higher threshold of missed visits would disproportionately select families with older children. We chose 2 or more missed well-child visits as the cutoff in order to include caregivers of young children as well as those of older children. We selected a purposive sample of 17 caregivers and 6 clinicians (family practice and pediatric physicians) for children aged 0 to 6 years who missed 2 or more well-child visits at Virginia Commonwealth University Health System (VCUHS) between January 1, 2011, and January 1, 2016. We aimed to assess current US caregiver and clinician perspectives regarding missed well-child visits in an urban, underserved health care system with a large proportion of African Americans. It is also unclear whether clinician and caregiver perspectives on missed well-child visits align. 10 Because clinicians are not always aware of the nonmedical aspects of patients’ lives, they may not fully understand or may have different perspectives on why well-child visits are missed. Clinicians in England also identified social reasons and family belief systems as reasons. Studies conducted more than 15 years ago identified transportation, 8, 9 work, 9 wait times, 8 and lack of understanding about the reason behind the visits 8 as reasons for missed visits. Despite these efforts, it is not fully understood why more disadvantaged patients miss a disproportionately larger share of well-child visits.įew studies have explored patient and clinician perspectives on why pediatric visits are missed. 5– 7 Many states support safety-net practices to promote access.

3– 6 Poor, uninsured, and African American children miss a greater proportion of these visits compared with upper-income, privately insured, and white counterparts. 3, 4 Despite these benefits, children miss between 30% to 50% of well-child visits. 2 Attendance of well-child visits has been associated with reduced hospitalizations and emergency department use. 1 These visits are an opportunity to deliver immunizations, provide anticipatory guidance, and identify and treat disease.

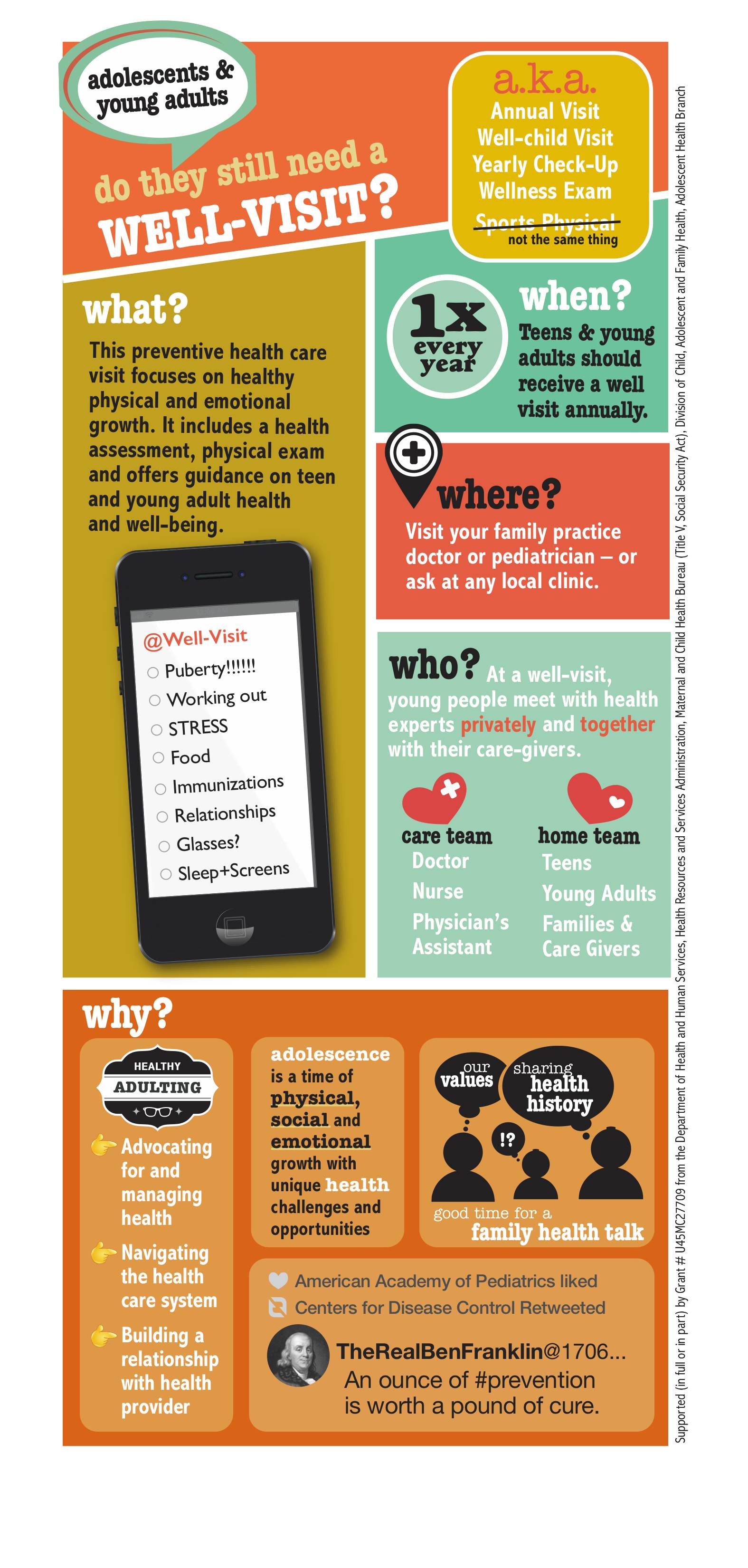
The American Academy of Pediatrics recommends 13 well-child visits before the age of 6 years.


 0 kommentar(er)
0 kommentar(er)
